adult RSV vaccine effectiveness/concerns
a
new report found that the respiratory syncytial virus (RSV)-related
hospitalizations and emergency department visits decreased dramatically with
the new RSV vaccination in high-risk adults aged 60 years or older (see rsv
vaccine effectiveness JAMA2024 in dropbox, or
doi:10.1001/jamanetworkopen.2024.50832)
Details:
-- 7047 patients with low respiratory tract disease
(LRTD)-related hospitalizations or emergency department (ED) encounters were
included in this retrospective case-control study with a test negative design
to assess the effectiveness of RSV vaccination, in the Kaiser Permanente
of Southern California (KPSC) database, from 2023-2024
-- KPSC includes 4.8 million members, with 11.1 being at least 60yo
-- RSVpreF vaccination (Abrysvo) was assessed during the first RSV season after vaccine licensure and 21 or more days before LRTD
--
cases: patients who were RSV-positive with LRTD events
--
controls (2 prespecified cohorts):
-- "strict controls" (primary analysis): LRTD events that were
negative for RSV, human metapneumovirus (HMPV), influenza, and SARS-C0V-2
(vaccine-preventable diseases); and they were positive for a nonvaccine
preventable disease comprising adenovirus, coronavirus (229E, HKU1,NL63, or
C43), human rhinovirus/enterovirus, parainfluenza 1-4, Chlamydia pneumoniae,
and Mycoplasma pneumoniae
-- this strict control was established to control for bias
associated with vaccine preventable disease and for the potential vaccine
effectiveness against HMPV (though there is no direct vaccine to prevent HMPV)
-- "broad" controls: RSV-negative LRTD events, regardless of
other identified causes (and also including those testing negative for all
pathogens)
-- this broad control was used as a more-encompassing
sensitivity analysis
--
in addition, there was "enhanced specimen collection", salvaging
clinical respiratory swabs not tested for RSV during routine care (ie,
respiratory specimens assessed specifically for SARS-CoV-2 and influenza that
were later found and retested for RSV)
-- salvaged specimens were more often from earlier in the
season and mostly done in non-Hispanic white patients,
those with few comorbidities, those who had the fewest health care
encounters in the prior year, and those presenting to the ED
--
mean age 76.8 years (57% were at least 75yo); 3819 (54.2%) were female; 839
(11.9%) were non-Hispanic Asian or Pacific Islander, 2323 (33.0%) were
Hispanic, 1197 (17.0%) were non-Hispanic Black, and 2602 (36.9%) were
non-Hispanic White
--
998 (14.2%) were immunocompromised; and 6573 (93.3%) had 1 or more Charlson
comorbidities, 72% had at least 3
--
specific comorbidities: peripheral vascular disease 68%, COPD 50%, kidney
disease 42%, heart failure 37%, malignant neoplasm 17%, MI 16%, cerebrovascular
disease 14%, dementia 12%,moderate-to-severe liver disease 2%, AIDS/HIV 0.3%
--
diabetes: HbA1c at least 7.5% in 16%, <7.5% in 34%, no diabetes in 48%
--
other markers of poor health: at least 1 hospitalization in the prior year in
39% (with 18% having >1); at least 1 ED visits in prior year in 62% (with
38% having >1); outpatient visits 71% at least 10
--
immunocompromised: 998 patients (14%)
--
exclusions: non-RSVpre-F vaccine recipients (eg those getting Arexvy, a
different RSV vaccine, as noted below) or those who had receive the RSV vaccine
<21 days before the LRTD encounter (who may have had suboptimal
immunity from the vaccine)
--
main outcome: estimated RSVpreF vaccine effectiveness (VE) against first
episode of RSV-related LRTD hospitalization or ED visit.
-- Additional outcomes evaluated in this group included
RSV-related LRTD hospitalizations, RSV-related LRTD hospitalizations among
patients with high-risk chronic medical conditions, RSV-related LRTD ED events,
RSV-related severe LTRD hospitalizations (ie, supplemental use of oxygen) and
ED events
Results:
--
8085 patients (77% of the total) had a nasal or nasopharyngeal swab:
5639 of them were tested directly for RSV and 4236 had RSV testing
from salvaged specimens
--
7047 LRTD events had tested specimens (62%) and were included in the
analysis
-- most common LRTD diagnosis: pneumonia
--
623 of the 7047 (8.8%) tested positive for RSV
--
223 (3.2%) of the total population received the RSVpreF vaccine
-- those most likely to be vaccinated: non-Hispanic Asian or Pacific
Islander and non-Hispanic white patients, and those with at least 10
outpatient encounters in the year before LRTD
-- those least likely to be vaccinated: those with peripheral
vascular disease, COPD or diabetes
--
27 RSV cases had viral coinfection
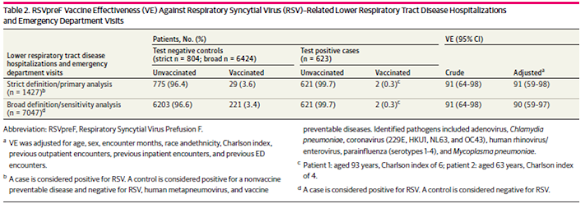
--estimated
adjusted VE using strict controls was 91% (59%-98%). Using broad controls,
estimated adjusted VE was 90% (59%-97%) [ie no difference]
other
findings: no difference in VE by LRTD hospitalizations or ED visits,
whether there were underlying high-risk chronic medical conditions, or severity
of RSV vaccination
Commentary:
--
prior studies have found RSV vaccine efficacy against LRTD, however the studies
had relatively few patients at least 75 years old or those with
comorbidities. This study was designed to assess a larger number of
patients who were sicker and had RSV-related hospitalizations and emergency
department visits
--
RSV infection in older adults is a common cause of severe respiratory disease.
In the US, 160,000 people at least 65yo are hospitalized for RSV
infections and 120,000 have ED visits annually
--
Notably, RSV infections can be associated with an increased risk of acute
cardiac events: a study in 2024 found that of 6248 patients hospitalized with
an RSV infection, 22% had an acute cardiac event (mostly acute heart
failure, in 16%), which happened much more so in those with underlying
cardiovascular disease, a group that also had twice the risk of severe
outcomes: https://pubmed.ncbi.nlm.nih.gov/38619857/ and
https://www.sciencedirect.com/science/article/pii/S0735109718304856?via%3Dihub
--
on June21, 2023 the FDA approved a single dose of this RSVpreF
vaccine (Respiratory Syncytial Virus Perfusion F) for people at least
60yo, with shared decision-making. the FDA was apparently hesitant
to have a stronger recommendation because of lack of vaccine effectiveness
regarding RSV-related hospitalization and among high-risk groups. Hence this
study...
--
current FDA recommendations were updated in 2024 to include all people 75yo or
older
--
there are 3 approved RSV vaccines (https://www.cdc.gov/vaccines/vpd/rsv/hcp/older-adults.html):
-- Arexvy: From GSK,
FDA approved May 2023: a recombinant RSV F protein antigen, stabilized in
the prefusion conformation (preF), and with AS01E adjuvant,
based on the RSV-A subtype
-- mResvia: From
Moderna, FDA approved in May 2024, a recombinant RSV F protein antigen,
stabilized in the prefusion conformation (preF), based only on the RSV-A
subtype
-- Abrysvo: From
Pfizer, FDA approved May 2023, nucleoside modified mRNA encoding the RSV F
glycoprotein, based on both the RSV-A and RSV-B subtypes
--
these vaccines can be administered with one or more other vaccines at the same
visit, though there might be increased local or systemic reactogenicity
(however, effectiveness data are mixed on the co-administration with influenza
vaccine)
--
so, what are the differences between the vaccines:
-- Abrysvo (the one used in this study) is based on both RSV types;
Arexzy and mReservia are based only on RSV-A subtype
-- But Arexvy does provide protection against both RSV A
and RSV B serotypes in some studies
-- mReservia did not have much effect on people >75yo in a phase 3
trial, and had an 80% decrease in hospitalization for RSV-associated
illness
-- Arexvy, per the FDA has an 83% decreased risk of developing
RSV-associated LRTD
-- for FDA info on the Arexvy and Abrysvo, see https://www.cdc.gov/acip/grade/protein-subunit-rsv-vaccines-older-adults.html; for
mResvia, see https://www.cdc.gov/acip/grade/mrna-rsv-vaccine-older-adults.html
-- BUT, one should be careful to actually compare these numbers
directly, since the studies are not direct comparisons and, for each vaccine,
there were different groups of patients with different diseases/disease
severities, etc
-- and, there is zero likelihood of a strong, well-designed randomized
controlled trial to see which vaccine is the best for which person (which might
vary based on the 2 groups: 60+ yo with comorbidities, and everyone at least
75yo); there may well be a best vaccine, but the other 2 drug
companies would not like to see those results!!!! could affect their
"bottom line".......
-- though, perhaps most significantly, mReservia is the only one with a
pronounceable name
-- then there is the issue of adverse effects of the RSV vaccines (https://www.cdc.gov/mmwr/volumes/73/wr/mm7321a3.htm#T3_download):
-- the current study above did not list (or likely have information)
about adverse effects in this retrospective study
-- the FDA report that compared Arexvy and Abrysvo found that the
minor adverse effects of Arexvy and Abrysvo were pretty similar overall
but the injection-site problems were more prevalent with the former
-- and there is that big issue of Guillain-Barre Syndrome (GBS):
"Among the 28 reports of GBS after vaccination that met case definition,
13 (46.4%) were after GSK vaccine Arexvy (1.8 reports per 1 million doses
administered), and 15 (53.6%) were after Pfizer
vaccine Abrysvo (4.4 reports per 1 million doses administered)
among persons aged ≥60 years. no info on the mReservia vaccine. of course, GBS
is quite rare, but still a bummer to get
--this
study affirms that in a sick patient population of people >60yo (57% being
>74yo), RSV infection was >90% effectively reduced by the RSVpreF
vaccine (the above results found that those with comorbidities the same
90% vaccine effectiveness, but the numbers of patients vaccinated in this study
who got documented RSV infections was small and non-vaccine studies have found
that those with more comorbidities getting RSV infections do worse: eg https://pubmed.ncbi.nlm.nih.gov/37970679/ ).
--
this overall result was similar to the prior clinical trial RENOIR with
the same RSVpreF vaccine (https://www.nejm.org/doi/full/10.1056/NEJMoa2213836 )
of those >60yo in those but with much less severe comorbidities, finding a
67% decrease in those developing RSV infection having at least 2
signs/symptoms of RSV and 86% for at least 3 RSV symptoms (ie, similar
decrease in patients getting more severe RSV infection of about 90% with
vaccination, but also very few cases assessed); adverse effects were
minimal and mild, related to the injection itself
Limitations:
--they
did include remnant swabs from patients who were tested for influenza and
covid, since the overall testing for RSV was quite low in their strict
analysis. this could introduce an important bias, since the group tested for
covid or influenza may be different than in a randomized trial (were they
sicker than those not considered for this testing?, did they present with
different symptoms??), though their findings by incorporating this large group
of patients did not change the results
-- that being said, the numbers of patients who were hospitalized with
RSV who had received the vaccine was really small (13 in total, which might be
related to the later rollout of RSV vaccination at KPSC)
-- and not all patients with LTRD had RSV testing (38% of LRTD patients
were not included in the study), again potentially distorting the results (was
it only the really sick ones who were tested??)
--
they only used the RSVpreF (after all, this was a drug company sponsored
study.....), so unclear if results pertain to the other RSV vaccines
--
this study did try to deal with the issue of the results being contaminated
from other vaccine-preventable infections, though we do know that there are
multiple viruses involved simultaneously in respiratory viral infections pretty
often. The numbers of infections overall in this study were too low to get
accurate information on the results of vaccination in those with multiple viral
infections vs just RSV: 27 of the 223 patients (12%) had RSV plus another viral
infection, muddying the waters a bit
--
overall, there is a quite low sensitivity of nasopharyngeal/nasal swab reverse
transcription PCR testing in adults (about 50% of RSV cases are not detected).
why was this so low? was it from poor technique? or characteristics or quantity
of the virus? how would this affect the generalizability of the results, since
the sensitivity of the PCR is so low?
--
this was a quite sick population with many comorbidities and lots of health
care encounters in the year prior to the study onset. this might not reflect
the effectiveness of the vaccine in less sick patients, despite their findings
otherwise
-- eg, some of the comorbidities included very few people (only 23 with
HIV/AIDS and 2 in the strict analysis; only 120 with moderate or severe liver
disease and 9 in the strict analysis), limiting generalizability to these
patients
—
the enhanced group of salvaged specimens did not reflect the specifics of the
overall group and could distort the results (they were more often assessed earlier
in the season, mostly in non-Hispanic white patients, those with few
comorbidities and those who had the fewest health care encounters in the prior
year); this enhanced group included 43% of the total
--
only 223 (3.2%) of the total population received the RSVpreF vaccine. the
results would be more rigorous in a larger study, especially given the above
concerns about their generalizability to the overall population
-- and the distribution of those vaccinated did vary by demographics and
comorbidities, again raising issues of generalizability
so:
--
despite the above-noted limitations, it does appear that the RSV vaccines are
really quite potent in preventing bad outcomes of RSV-associated lower
respiratory tract disease
--
as with all vaccines, there are relatively frequent local adverse effects at
the site of the injection, with a very rare likelihood (though should be
mentioned to patients...) of Guillain-Barre syndrome, and the incidence of GBS
seems to be in-line with influenza vaccine (per the CDC, "The data on
the association between GBS and seasonal flu vaccination are varied and
inconsistent across flu seasons. If there is an increased risk of GBS following
flu vaccination, it is small, on the order of one to two additional GBS cases
per million doses of flu vaccine administered")
--
there is a significant mortality from RSV infection in adults >60yo, perhaps
in the 9% range for hospitalized patients (https://pmc.ncbi.nlm.nih.gov/articles/PMC10911257/)
-- so, the perspective is that LRTD can be a very severe or fatal in
RSV-associated infection, statistically supporting the use of the vaccine in
those at high risk for these complications
--
and, it seems it is a one-time injection (at least for now)
--
also, by the way, the CDC also recommends that the Abrysvo vaccine (no mention
of the others) be given to pregnant people during 32-26 weeks of pregnancy, to
protect the infant (earlier immunization is discouraged because of waning
antibody titers passed to the neonate)
geoff
-----------------------------------
If you would like to be on the regular email list for upcoming
blogs, please contact me at gmodest@bidmc.harvard.edu
to get access to all of the blogs: go to http://gmodestmedblogs.blogspot.com/ to
see the blogs in reverse chronological order
or you can just click on the magnifying glass on top right,
then type in a name in the search box and get all the blogs with that name in
them

Comments
Post a Comment
if you would like to receive the near-daily emails regularly, please email me at gmodest@uphams.org