chronic prostatitis/chronic pelvic pain syndrome: acupuncture helps
A Chinese randomized trial found that acupuncture helped men with
Chronic Prostatitis /Chronic Pelvic Pain Syndrome (CP/CPPS): see acupuncture
helps chr prostatitis/chronic pelvic pain in men AIM2021 in dropbox,
or doi:10.7326/M21-1814
Details:
-- 440 men from 10 tertiary hospitals in cities across China were
randomized to real acupuncture versus sham acupuncture
-- acupuncture was applied in the standard
manner with needles inserted to a depth of 25 to 30 mm at the designated
acupuncture sites, accompanied with gentle and even manipulations once every 10
minutes, 30 seconds at a time
-- sham acupuncture involved using minimally
invasive needles inserted 2 to 3 mm at non-acupoints, without manipulation
-- patients were given 20 sessions over 8
weeks, with follow up 24 weeks after
treatment ended
--all patients were 18 to 50 years old, and scored at least 15 on
the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI)
-- the NIH-CPSI is a universally accepted, reliable,
and valid instrument recommended in consensus guidelines, which measures pain
(score 0-21), urinary function (0-10), and the effect on quality of life (score
0-12), with a total score ranging from 0 to 43, higher scores being worse
-- a 6-point decrease in the total score is
considered a clinically important improvement
-- this instrument was used at weeks 8 and 32
(24 weeks after finishing treatment)
-- mean age 36, BMI 24, median sexual frequency once per week,
current smoker 37%, current drinker 53%, sedentary life 70%, median CP/CPPS symptom duration was 2 years
-- mean peak urinary flow rate 22 mL/s; mean average urinary flow
rate 12.5 mL/s; median total PSA 0.6 ng /mL; median residual urinary volume
4ml
-- prior therapies: herbal medicine 35%, local treatments 11%,
antibiotics 8%, alpha blockers 5%, physical therapy 3%, 5-alpha reductase
inhibitors 2%
-- NIH-CPSI mean was 31, with subscales:
-- pain subscale: 17 (range 0-21)
-- urinary subscale: 5 (range 0-10)
-- quality-of-life subscale: 9 (range 0-12)
-- 78% of patients believed that acupuncture “is effective for
treating diseases in general” and 71% thought “it will be helpful to
improve your CP/CPPS symptoms”
-- primary outcome: proportion of participants who achieved a
clinically important reduction of at least 6points from baseline in the
NIH-CPSI at weeks 8 and 32
-- secondary outcomes: evaluation for quality of life (EuroQol 5
Dimension 5 Level, minimally clinically important difference between
0.03-0.05), the Hospital Anxiety and Depression Scale (HADS, minimally
important difference 1.7 points),
the International Prostate Symptom Score (IPSS, minimally important difference
was 5.2), and urologic measures of peak and mean urinary flow rates
Results:
-- response at week 8 (at end of acupuncture sessions), with
response defined as a reduction at least 6 in NIH-CPSI:
-- acupuncture: 60.6% (53.7%-67.1%)
-- sham acupuncture: 36.8% (30.4%-47.3%)
-- adjusted difference 21.6 percentage points
(12.8-30.4 percentage points), adjusted OR 2.6 (1.8-4.0), p<0.001 (adjusted
scores were for the baseline NIH-CPSI total score)
-- response at week 32:
-- acupuncture: 61.5% (54.5%-68.1%)
-- sham acupuncture: 38.3% (31.7%-45.4%)
-- adjusted difference: 21.1 percentage points (12.2 - 30.1 percentage points), adjusted odds ratio 2.6
(1.7-3.9), p<0.001
--marked or moderate improvement, acupuncture vs sham acupuncture:
--week 4: 39.9% vs 22.1%
--week 8: 67.0% vs 36.5%
--week 20: 48.5% vs 24.5%
--week 32: 47.1% vs 25.0%
--marked improvement
-- week 4: 15.9% vs 7.5%
-- week 8: 30.6% vs 8.7%
-- week 20: 24.3% vs 6.7%
-- week 32: 22.3% vs 8.2%
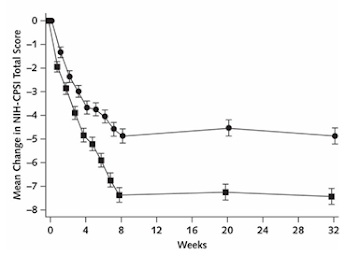
Mean
change in NIH-CPSI total score from baseline (top=sham acupuncture;
bottom-=real acupuncture); treatment ended at week 8
other
outcomes:
--
NIH-CPSI subscales at week 32, adjusted difference of acupuncture vs sham
acupuncture:
-- pain: acupuncture: -2.0 (-2.3 to -1.8) vs sham -1.3 (-1.5 to -1.0),
adjusted difference -0.8 (-1.1 to -0.4)
--urinary: -2.1 (-2.4 to -1.9) vs sham
-1.5 (-1.8 to -1.2), adjusted difference -0.6 (-1.0 to -0.3)
--quality of life: -3.1 (-3.5 to
-2.8) vs sham -2.1 (-2.4 to -1.8), adjusted difference -1.1 (0-1.5
to -0.6)
--
adjusted mean change in average urinary flow rate at week 32: 0.5 mL/s
for acupuncture and -0.24 mL/s for sham acupuncture
--
adjusted mean change in peak urinary flow rate: at week 32: 0.5 mL/s for
acupuncture and -0.64 mL/s for sham acupuncture
--
mean change in IPSS score at 32 weeks: -4.7 versus -3.1
--
mean change in HADS score at week 32: -2.8 versus -0.5 (higher scores indicate
more anxiety and depression)
--
mean change in EQ-5D-5L score at week 32: 0.06 for acupuncture, 0.03 for sham
agriculture (higher score reflecting better generic health status)
--
No serious adverse events reported
Commentary:
--
CP/CPPS can be a disabling condition involving urogenital pain, lower urinary
tract symptoms, psychological issues, and sexual dysfunction
--
studies suggest that 2 to 16% of the male population of high-income countries
and 11% in lower- and middle-income countries have this disorder
--
studies have also shown that the negative effects on quality of life from
CP/CPPS are on the order of those from angina, MI, heart failure, diabetes, and
Crohn’s disease
--
the purported mechanism of CP/CPPS is some combination of inflammation in the
prostate, anxiety, stress, and dyssynergic voiding
--
treatment with antibiotics (mostly for those with positive urine cultures and
symptoms consistent with cystitis), alpha blockers, and anti-inflammatories are
used in clinical practice but do not have much benefit over placebo (and much
less than the acupuncture ones above), and any effect fades after the
medication is discontinued
--
prior studies on acupuncture have not been of high quality, though a 2018
Cochrane review of nonpharmacological interventions in treating CP/CPPS
(doi:10.1002/14651858.CD012551.pub3) did note that only acupuncture and
extracorporeal shock wave therapy were likely to result in symptom relief with
a good safety profile
--
this study found that acupuncture did have significant and durable effects for
24 weeks after the end of treatment, in a group of men who had had these
symptoms for a median of two years, scored
pretty high on the NIH-CPSI scale, and many had tried different
prior therapies
--
it was impressive that there was no falloff in improvement in either
acupuncture group from 8 weeks to 32 weeks
--
all of the NIH-CPSI subscales showed improvement (other than sexual
dysfunction)
--
and, all of the scores around anxiety, depression, quality-of-life were better
with acupuncture, though some did not reach clinically meaningful significance
--
one question is why did sham acupuncture work so well. Part of the issue may be
that these patients were predisposed to feeling that it would help (71% thought
acupuncture would help their symptoms) leading to an augmented placebo effect
for both real and sham acupuncture. In addition, it is possible that sham
acupuncture itself might have a clinical benefit:
--
this study did find that although the net change from baseline was more than 7
points in the acupuncture group, the sham
group was pretty close at about 5 points at weeks 8 and 32; ie, the
acupuncture group did reach a clinically meaningful difference, though the
difference between the achieved benefit in both groups was less than three
points (which is less than the 6-point clinically meaningful difference).
--
The reason for the closeness of these two results could be a few things: the
placebo effect of the sham acupuncture or perhaps there was an actual benefit
from sham acupuncture, as noted, or perhaps that this average response did not
reflect a significant skew in benefit. For example, perhaps actual acupuncture
led to dramatic benefit in a significant subpopulation of patients (for unknown
reasons), yet there were many who did not respond, leading to a less impressive
average for the group.
--
Also, there may be significant differences in the approach and biases related
to the acupuncturists for each group, who clearly knew which patient was in
which group. Acupuncture does involve an intimate interaction between the
clinician and patient, which might lead to a different placebo effect in the 2
acupuncture groups. and, as we know in primary care, the relationship itself is
often clinically therapeutic. And this may be why the acupuncture results were
better than our typical medication approach.
--
acupuncture does have some pretty clear physiologic effects: release of central
opioid peptides (enkephalins, endorphins, dynorphins), with their attendant
analgesic and euphoric effects; anti-inflammatory effects (inhibiting
cyclooxygenase synthesis and peripheral and central nociceptive sites, eg see https://www.nature.com/articles/s41586-021-04001-4 );
and inhibiting prostaglandin E2 release, which is highly expressed in patients
with CP/CPPS, (see acupuncture dec prostaglandin E2 in chronic
prostatitis urol2009 in dropbox, or doi:10.1016/j.urology.2008.10.047)
Limitations:
--
the methodology of acupuncture versus sham acupuncture seems to me to be quite
different, with the true acupuncture needles being inserted much more deeply
and with manipulations, versus the sham acupuncture with only superficial
insertion without manipulation. Not sure if this would clue people to knowing
which group they were assigned to (though those in the sham group did quite
well...)
--
and, as alluded to above, the attitude and sense of intimacy with patients may
be different when an acupuncturist was convinced that they were doing real
acupuncture (which the acupuncturist might have felt strongly would be
beneficial) versus those doing very superficial needling of patients, where the
acupuncturist might then have less of an intimate relationship and might create
less of a feeling of hope for the patients (though, again, the sham group did quite well, but ??might have done better??)
--
this is a group of patients who were very attuned to acupuncture, and had a
very positive outlook on its potential. This may not be generalizable to other
populations
so,
pretty impressive. acupuncture might really have a place in the treatment of
this difficult and not-so-uncommon problem, especially given the apparent
inadequacies of many of our current approaches. one concern, or course, is the
acceptability and anticipation about acupuncture effectiveness in Western
societies. My limited and skewed practice (largely immigrants from central america
and cape verde) has found great acceptance and benefit from acupuncture when it
was available at our health center. Maybe if presented in a strongly positive
way, it would be generally acceptable (more like: "do i have a great
option for you...")
geoff
If you would like to be on the regular email list
for upcoming blogs, please contact me at gmodest@uphams.org
For access to the dropbox, go to link: https://www.dropbox.com/sh/0bmvtita8mzms11/XDTwHySFFg
to get access to all of the blogs (2 options):
1. go to http://gmodestmedblogs.blogspot.com/ to see them in reverse chronological order
2. click on 3 parallel lines top left, if you
want to see blogs by category, then click on "labels" and choose a
category
3. or you can just click on the magnifying
glass on top right, then type in a name in the search box and get all the
blogs with that name in them
or: go to https://www.bucommunitymedicine.org/ ,
a website from the Community Medicine section at Boston Medical Center.
This site does have a very searchable and accessible list of my blogs (though
there have been a few that did not upload over the last year or two). but
overall it is much easier to view blogs and displays more at a time.
please feel free to circulate this to others.
also, if you send me their emails, i can add them to the list

Comments
Post a Comment
if you would like to receive the near-daily emails regularly, please email me at gmodest@uphams.org